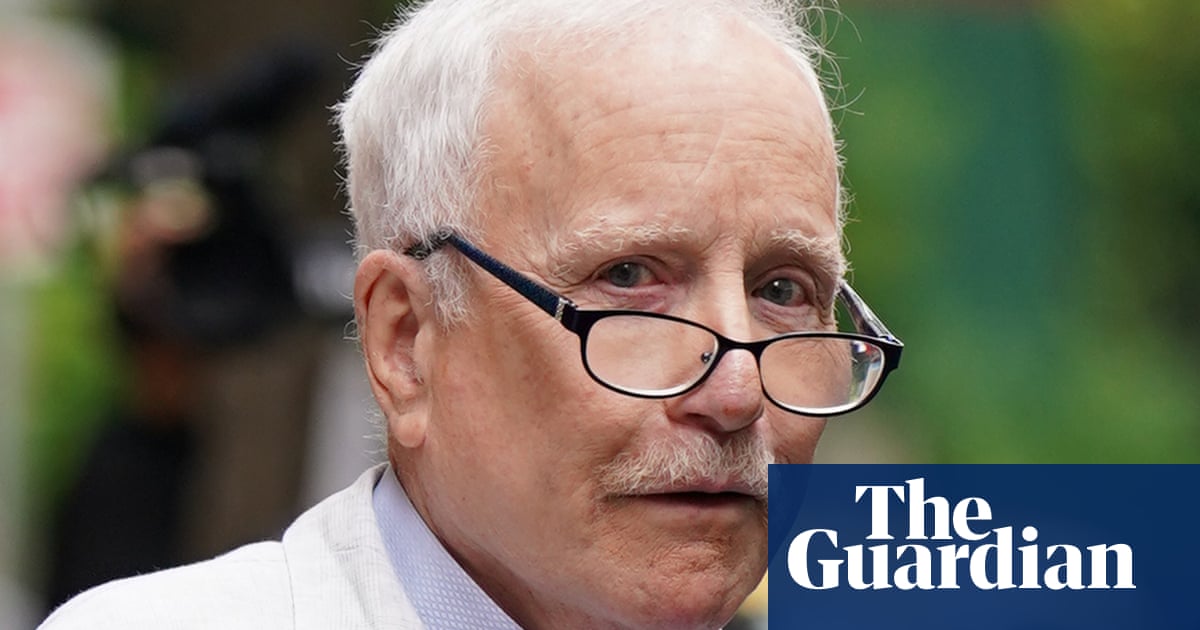
In February, my partner, Henry McDonald, who wrote for this newspaper, lost his fight with cancer. I say “fight” because those were his words and, as a journalist, Henry chose them carefully. Reporting on the Troubles in Northern Ireland for more than two decades, and some of the worst atrocities that befell this part of the world, he knew more than most that words mattered. Above all, Henry stood up for those without a voice – the victims.
In the UK, doctors are failing to do the same for patients. Henry was one of them. Across this country, most patients still don’t have access to their online medical records. Many doctors are against allowing it. As part of the new GP contract, NHS England announced early in March that all patients accessing primary care should be offered access to their online records, via the NHS app and other portals, by October. The British Medical Association opposes the move, marking yet another delay in an endless saga.
Doctors seem to think patients like Henry, who had survived multiple paramilitary death threats, lack the emotional fortitude or capacity to read about their own health. Despite progress in England, four in five primary care practices still fail to offer online access – and because few British hospitals have digitised their health records, online access to specialist care is beyond the realm of the possible.
GPs worry about this radical change, fearing additional burdens for their work and an onslaught of calls or emails from anxious and confused patients. They cite risks to patients’ safety and legal woes as their reasons for resistance.
However, the experience in other countries challenges their concerns. Patients in Estonia, Finland, Norway and Sweden have been granted secure online record access for years – in some regions, for more than 15 years. In April 2021, the US followed suit: the 21st Century Cures Act mandated that all patients should be offered online access to their full clinical records without charge. Patients can now read their primary care and hospital records, and even test results, online. Doctors were cynical in these countries too, but after access the sky didn’t fall in. Patients could be “trusted” to read their own information. Meanwhile, the benefits to patients are legion: better understanding and remembering what the doctor said – and feeling more engaged with, and in control of, their health.
Henry was first treated for stomach cancer in 2018. With each passing season, he seemed healthier and stronger, his febrile energy returning. He published a second novel, completed a third, and ghostwrote a political memoir, all while continuing in frontline journalism. We dared to believe that he would soon achieve the milestone of being cancer-free for five years.
Last September, Henry’s health took a serious downturn. He was admitted to hospital for what doctors believed was a gallbladder problem, then sepsis. Henry moved wards and then hospitals, and was seen by multiple teams and specialists. Although his care was truly excellent, in Henry’s own words, “the communication was appalling”.
Some doctors seemed diffident about divulging the facts, preferring to speak in infantilising euphemisms. At one early visit, Henry – who quizzed politicians and terrorists for a living – was informed by a specialist: “This could be a bad thing or a very bad thing.” At the other extreme was a tendency to hide behind impenetrable medical jargon. Of course, there were rare exceptions: Henry credited one of his doctors as particularly lucid in explaining complex medical facts and giving it to him straight. But even in this best-case scenario, the flow of information was spluttering and sporadic.
Throughout his illness, unlike patients in other countries, Henry never had immediate access to his numerous test results and what they meant. Since most clinical conversations took place when Henry was utterly exhausted after yet another night of broken sleep on the ward, he struggled to recall everything the doctors said. As a trained journalist, Henry could use shorthand, but life-or-death medical conversations are not the place for detached jottings. Because many of these meetings happened outside visiting hours, neither I nor Henry’s family could be there to take notes or ask questions.
The upshot was that Henry, and in turn, we – his loved ones – were often in the dark, struggling to piece together fragments of secondhand information. At an already stressful time, lack of access only exacerbated the distress.
Doctors seldom stop to consider the harms this way of working causes patients, preferring instead to overestimate their own priestly role in medical conversations. Studies of patient experience offer stark home truths. In countries that have made the transition, such as Sweden, patients with cancer say transparency is crucial for their mental wellbeing and to help them prepare for appointments. In the US, a staggering 95% of patients say they prefer bad news to no news – even if it means reading test results online before talking with a doctor.
Lack of access also created confusion. After weeks of medical examinations, one doctor told Henry he was “cancer-free”. Was this a medical miscommunication? Did Henry misinterpret what was said? Yet he was utterly adamant those were the words used. With online record access we might have been in a better position to query this, or at least ask if all the test results were in yet, avoiding another rollercoaster of distress.
Two months before he died, Henry’s medical team pulled the blue curtains round his hospital bed. The doctor spoke with compassion and candour, albeit within earshot of the other patients on the ward, to tell us Henry’s stomach cancer had returned. It would not be treatable. Even in this – the worst of all possible scenarios – lack of access cast a shadow. “The present medical situation,” we were told, “began in February.” February? Was there a crucial test result we didn’t know about? We were at a loss about what this meant.
Henry was angry. He was also stoical and practical, and exercised his legal right to request copies of his medical records to seek second opinions. The medical staff were amenable, but it took almost four weeks to obtain copies. Nor did we blame the clinicians: we recognised the pressures they worked under. We knew they could probably have done without our constant emails. Then again, how else were we to access Henry’s records?
We finally obtained them – via post. As we did not own a scanner, a friend volunteered to convert them into pdfs so we could send them to other clinics via more modern but less secure methods – ie email. We immediately felt slightly more in control of an already dire situation. We pursued our medical contacts in the US and the Republic of Ireland. Nothing could be done. But we knew we’d tried everything.
Henry was intensely trusted as a journalist in our troubled corner of the world, because he stood up for justice and the facts, and didn’t underestimate his readers. He never caved into tribalism or romancing about the past. If only the medical profession could be more like him.
Charlotte Blease is a research affiliate in digital psychiatry at the Beth Israel Deaconess Medical Center, Harvard Medical School and at the Department of Women’s and Children’s Health, Uppsala University

 1 year ago
60
1 year ago
60








 English (US)
English (US)